Our claims management software has intuitive functionality that optimizes workflow, reduces errors, and accelerates cash flow. Edit and submit Institutional and Professional claims to Medicare, Medicaid, Blue Cross plans, and commercial insurance companies; retrieve payer reports; rework rejected claims. We tailor Claim Agent to your specialty and meet your business needs. To schedule a demo, please visit the Contact Us page and fill out the form or give us a call.
Import
Import
Import claim files from any practice management and billing system
Repair
Repair
Edit Claims accurately and efficiently with our extensive validation checks
Submit
Submit
Submit ANSI 837s and 276s to payers, clearinghouses, and financial systems
Retrieve
Retrieve
Retrieve acknowledgement files, ANSI 835s and ANSI 277s
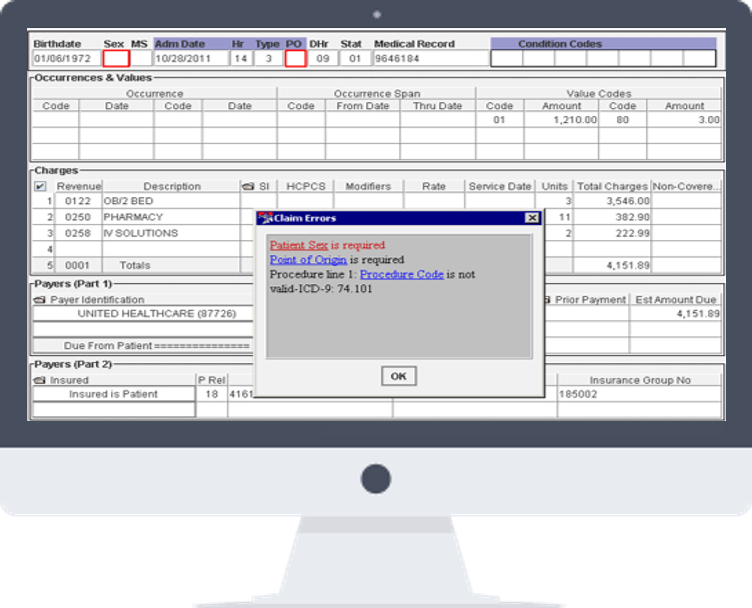
Claim Scrubbing
Clean Proficiently. Review How You Want.
Find and correct claim errors with our powerful and customizable rules engine. Claims are subjected to extensive edits that are personalized to the provider and payer. Multiple control points ensure that only clean claims are submitted.
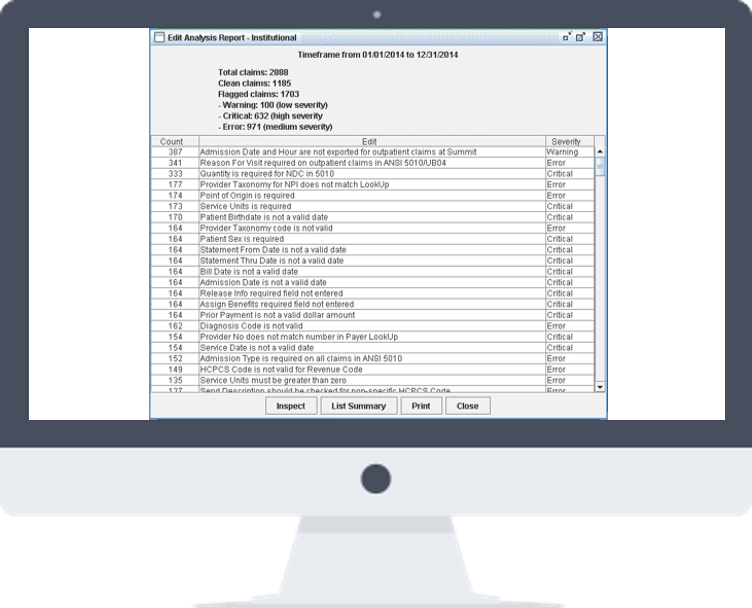
Data Analytics
Discover More. Find What You Want.
Claim Agent’s operational reports, management reports, productivity reports, and denial management reports provide valuable data about the claim, workflow, and employee productivity.
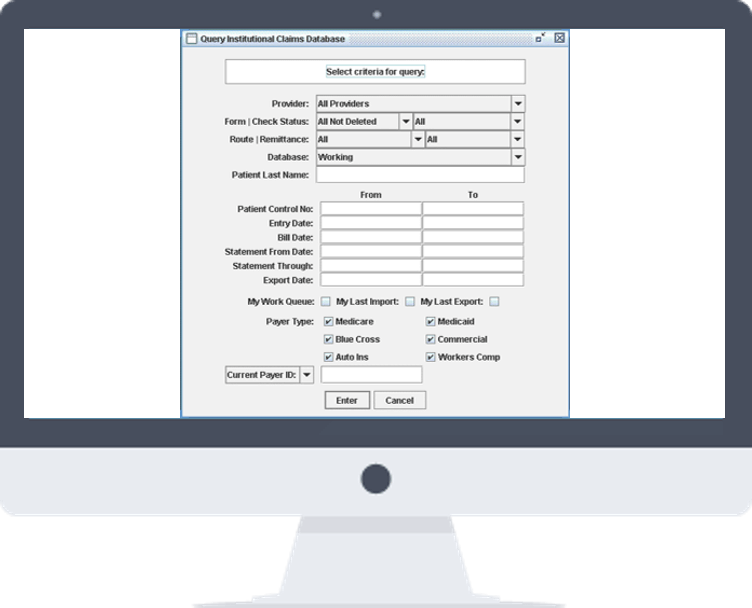
Claim Follow Up
Collect Faster. Manage How You Want.
Manage your secondary and rejected claims. Retrieve payer reports; track claims; create Ad Hoc Queries and Hold Reports. Our Remittance Matching tool automatically posts ERA to the billed claim and can create new claim for the secondary payer.
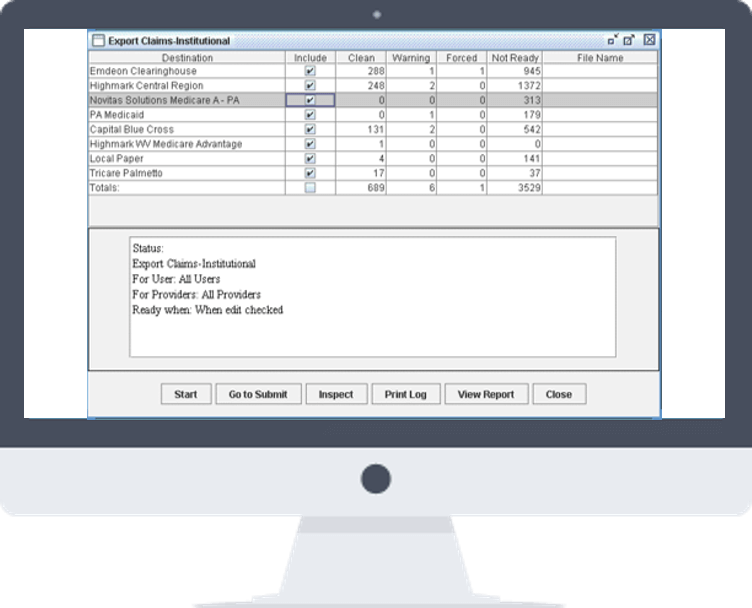
Electronic Data Interchange
Connect Securely. Send to Whom You Want.
Import and export ANSI 276, 277, 835, and 837 and print files. We designed Claim Agent to read our customers’ and payers’ files. It is compatible with any payer, clearinghouse and practice management system.
Additional Features
Privacy and Security
Meets and exceeds HIPAA requirements
Bridge Routines
Performs automatized tasks for the user
Help System
Assists you throughout the claims process
Audit Trail
All activities related to a claim are recorded
Work Flow
Utilize user settings to maximize output
Ad Hoc Queries
Explore all information within the database
